Hard(ware) To Say Goodbye
A traumatic injury is always accompanied by changes that need to be overcome, or at the very least, acclimated to. Even if no paralysis has occurred, victims of physical trauma often need to relearn basic skills as their body gets back into working order; relearning how to walk, how to get dressed, and how to remain hygienic are all common struggles that can affect a person who has spent any extended period of time in the hospital.
Another common hurdle to clear for patients overcoming a great injury is the subsequent healing period required after reparative surgery. Incisions, sutures, and staples must all be negotiated, to say nothing of external hardware that may have been temporarily affixed, like a chest tube, epidural, or a walker and crutches. All of these hallmarks of surgery will eventually be disposed of as the patient heals, however; staples will be removed, steri strips thrown away, and incision points will scar over. All that’s left is physical therapy, right? Unfortunately for many, the biggest long-term adjustment surrounds internal surgical hardware. Some of it is permanent, and some of it can be removed, at the request of the patient. Knowing when and if to remove internal hardware is a question that plagues patients who are tired of dealing with hospitals, therapists, and mounting surgery bills.
The Two Sides Of Orthopedic Hardware
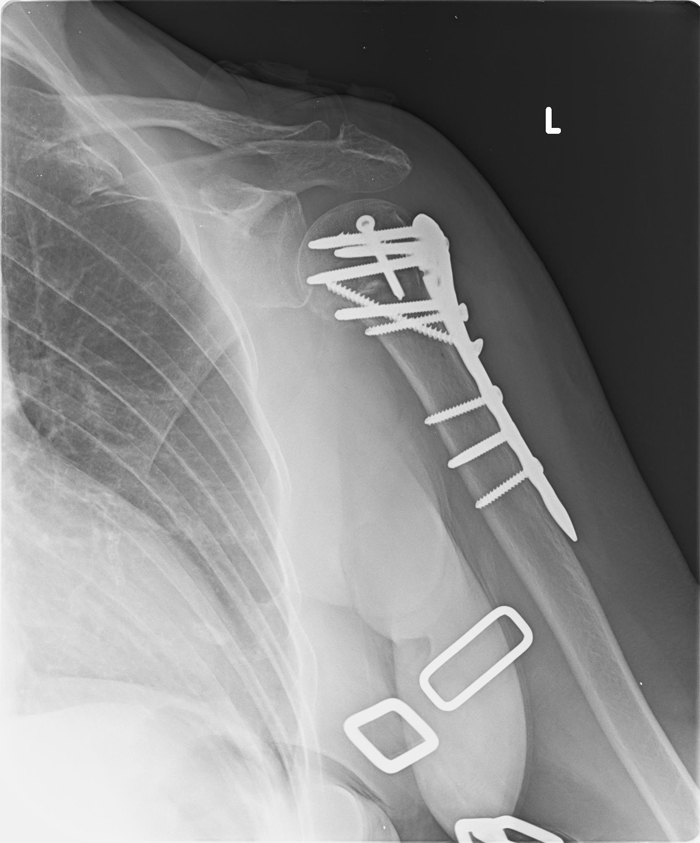
The question of whether or not to remove orthopedic hardware is a taxing one and even the best orthopedic surgeon can only advise. Pins, screws, plates, wires, and rods often carry the contradictory honors of strengthening and supporting broken bones, while also limiting range of motion or causing chronic pain for months and years to come. A shoulder surgeon might tell you that it’s okay to come back and remove a plate “if you want,” but how can a patient know when it’s the right time?
Recognizing that some hardware is permanent and the patient does not have the option to remove it, what are the pros and cons of taking action?
The Pros
There are a number of reasons why a person could be happy having their hardware removed. A few are obvious, and some not so much.
- A reduction in pain: Persistent pain after having hardware put in is not uncommon, as are swings in the pain intensity. Having that hardware removed is a way to deal with this issue head-on. Orthopedic surgeons have been known to remove plates and screws if any nerve damage has occurred around the site of the surgery.
- An aid to more complete healing: While plates, screws, and other instruments can support breaks until they have fused back together, an elbow or foot surgeon, for instance, may want to remove the gear if full range of motion hasn’t returned, or there were complications with the surrounding area’s ability to heal.
- It’s easier for hospital techs: This might be an obtuse reason for a patient to take out their hardware — it certainly isn’t up to them for hospital staff to be fully able to perform their jobs — but there has been dialogue between orthopedic surgeons and imaging techs. The latter often has a hard time assessing imagery of internal structures if there are plates or screws covering things up. If you find yourself going back often for check-ups, or are in a high-risk job where injury is possible, taking out the hardware could eliminate the potential of getting back a less-than-stellar assessment by techs who are still learning.
- It might be safer in the long run: According to studies, shoulder and elbow surgeons (among others) have opted to trade in stainless steel instruments for titanium. Over time metal in the body has the potential to corrode, or hamper natural growth of the affected bone or limb.
The Cons
It’s important to remember that any real cons to removing your surgical hardware will be discussed with you by your orthopedic surgeon. But there are a number of reasons why people would want to hold off from removing anything once it’s been put there.
- It’s extra recovery time: Surgery requires recovery time — that’s a fact of life. Depending on your age, weight, the seriousness of the original injury, and the extensiveness of the implant, recovery could take weeks, or longer.
- Removing could complicate your recovery: Anytime soft tissue is involved in surgery, there’s a chance that scarring will cause nerve damage, which could impair you forever. There’s also a chance that the weak area currently being supported by the hardware would fare poorly without that structure in there, should trauma occur again.
- Post-Op complications: There are also issues that can arise after any type of surgery. Infections, internal and external bleeding, and issues with completely removing long-embedded gear have been known to complicate matters.
The Orthopedic Surgeon Is Your Best Resource
The decision to remove surgical hardware is a complicated one that you will likely be thinking about for a long time. Your orthopedic surgeon will likely have the data (and certainly the experience) to advise you on your options. With the right medical team, your chances of lasting post-op complications go down significantly. That has got to feel good.